Three years had passed by. I seldom kept in contact with this pet shop girl till recently as I don't go to the shop to do puppy vaccinations. However, I visited to ask her to re-pack some Hill's Prescription d/d dog food for me as many owners want small packets.
Another aged female Cocker Spaniel of around 12 years old, belonging to her sister had open pyometra some months ago. The sister had put the dog on antibiotics for some time. "It is best to spay her," I advised. But the sister just would not want to. I don't know why.
Finally, the dog was operated by another vet and survived. "But I have to provide my dog (Golden Retriever) for blood donation as the platelet count was very low," the pet shop girl said when I visited her pet shop. That was good news. But there was a high cost involved.
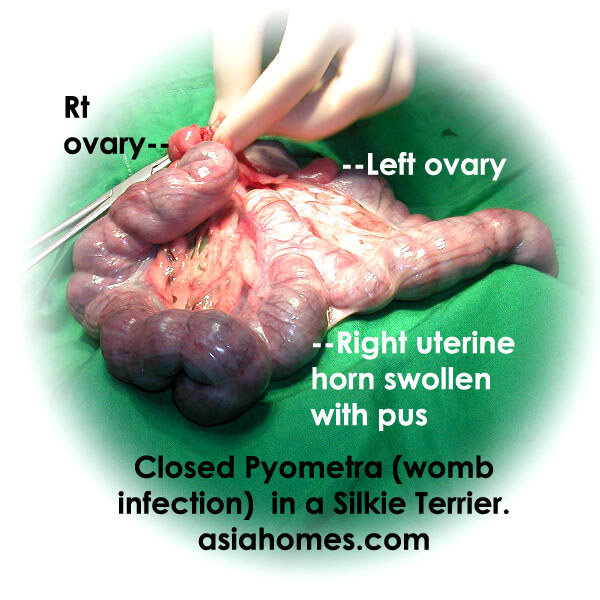
Spaying the female dog early would have prevented pyometra in these two cases which were not handled by me or my Surgery. As an alternative, inspect your female dog monthly. Record her dates when she has her heat. Observe the colour and nature of the blood spots. If the blood looks brownish or yellowish and starchy, it is time to get her spayed. Unfortunately, in closed pyometra, there are no discharge. Just vomiting. Or loss of appetite and lethargy.
It seemed a repeat of history during this visit. There was the pyometra of her sister's dog. There was also a slim teenaged girl working as a part-timer busy cleaning up the kennels at 11 am when I visited. However, this short girl was not thin She was OK and could be considered "handsome". But she had a ring in between her nostrils. Her unique selling proposition.
She reminded me of the bulls I saw practice as a 4th year vet student some 30 years ago in Scotland in 1973. Such bulls have a ring between their nostrils if my long-term memory is still intact. Why would such a young teenaged girl with normal good looks put ring her nose I just cannot understand. She hung with her friends past midnight at the Junction 8 shopping mall in Bishan and was working part-time to earn some money.
"Do you want to employ her as a part-timer," the pet shop girl asked me. "She can try out for one day without payment first."
"I need a girl who knows how to write reports and use the Excel and Microsoft Word," I told the pet shop girl. It is difficult to find such part-timers. I can't employ any nose-ringed girl or boy as part-timers no matter how hard working they are. Buttons embedded in the girl's tongue. Well, I don't know how such girls do it. It must be very painful. However times have changed for some young adults.
As for pyometra in aged female dogs, things have not changed much in the treatment or cure. Prognosis is poor when the owner delays veterinary treatment and when there is vomiting. Spaying would not be of much help once the female dog has persistent vomiting for several weeks as the kidneys had been damaged. Some 10 years ago, I had an uneducated owner bad-mouthing me for not curing the dog after the spay of her persistently vomiting dog. The dog survived the spay but continued vomiting due to kidney disease, not to professional incompetence of spaying! The lady owner did not want any blood test but the cheapest veterinary cost. Sometimes it is best not to handle such personalities who want "cheap and good" veterinary services if the vet cares about the reputation built up over the years. They tend to bad-mouth the vet in the Singapore internet forum nowadays and this webpage will persist forever for people all over the world to see.
For aged female dogs with pyometra, family members may get is the pain or in this case, the younger sister felt the pain of the suffering of the aged female dog.
For those who believe in prevention of pyometra, spay your female dog early, 3 months after the first heat.




































